High blood pressure is often called the “silent killer” because it damages the body without showing early warning signs. One of its overlooked effects is on vision, where it leads to a serious condition known as hypertensive retinopathy. This disease occurs when high blood pressure damages the retina, the light-sensitive tissue at the back of the eye. Without proper management, it can cause severe vision problems or even blindness.
That is why comprehensive eye disease management is essential. At Vision Gallery, we focus on preventive care, early diagnosis, and advanced treatment options to protect your eyes. By treating hypertension and monitoring eye health, long-term damage can be reduced. Early intervention ensures a higher chance of preserving healthy vision.
What is Hypertensive Retinopathy?
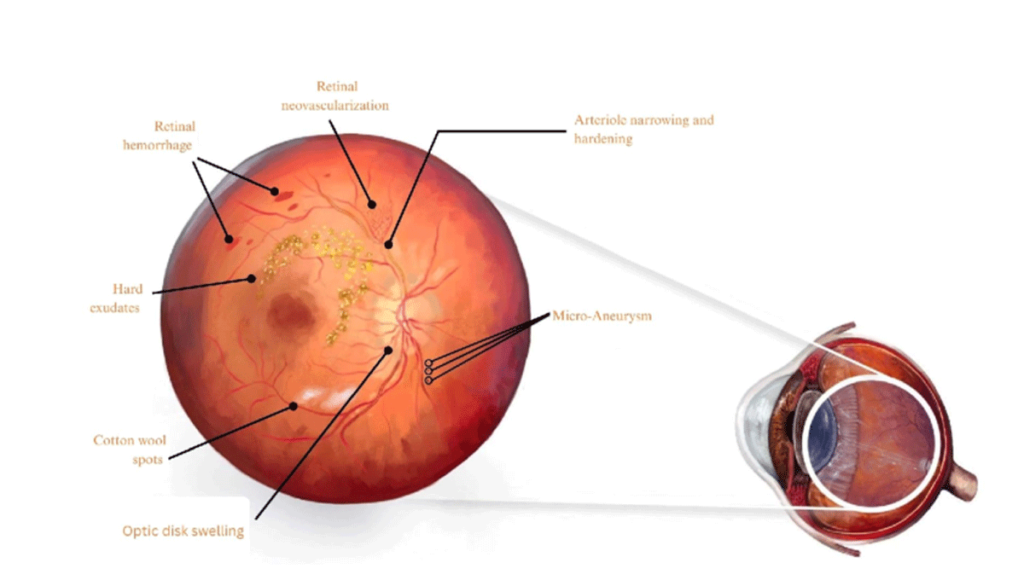
Hypertensive retinopathy occurs when long-term high blood pressure strains the delicate blood vessels in the retina. These vessels may narrow, leak, or become blocked, causing vision disturbances. Since the retina is vital for sending light signals to the brain, any damage can directly affect eyesight. The condition usually progresses silently, making regular eye exams crucial.
Key points about hypertensive retinopathy:
- Caused by high blood pressure damaging retinal vessels.
- Progresses gradually, often without early symptoms.
- Leads to blurred vision, swelling, or bleeding in the eye.
- Detected through detailed eye examinations.
Stages of Hypertensive Retinopathy
Hypertensive retinopathy progresses through different stages depending on how long and how severely blood pressure has been uncontrolled. Each stage shows distinct changes in the retina and determines the urgency of treatment. Understanding these stages helps patients recognize the importance of early detection and routine eye exams.
Stages include:
- Stage 1: Mild Retinal Vessel Narrowing
In the earliest stage, the small blood vessels in the retina become slightly narrowed. This change usually doesn’t affect vision and is only detectable during an eye exam. With proper blood pressure control, progression can often be prevented. - Stage 2: Moderate Retinal Vessel Changes
Blood vessels show more noticeable narrowing, and the arteries may begin to cross over veins abnormally (known as arteriovenous nicking). Vision is still often unaffected, but the damage indicates that hypertension is becoming more severe. Early treatment at this stage is very important. - Stage 3: Retinal Swelling and Hemorrhages
At this stage, the retina may show swelling, bleeding (hemorrhages), and cotton-wool spots, which are signs of reduced blood supply. Patients may start experiencing blurred vision or headaches. The risk of permanent damage to eyesight increases significantly. - Stage 4: Severe Retinal and Optic Nerve Damage
This is the most advanced and dangerous stage, where the optic nerve becomes swollen (papilledema). Vision loss can be severe, and it is often a medical emergency requiring urgent blood pressure control. Stage 4 is also associated with a higher risk of stroke and heart disease.
How Common Is This Condition?
Hypertensive retinopathy is more common than many people think. A large number of people with long-standing hypertension develop some level of retinal changes. The longer high blood pressure remains uncontrolled, the greater the risk becomes. This condition is especially prevalent in patients with other chronic diseases like diabetes and kidney disorders.
Facts about its occurrence:
- Common in adults over 40 with long-term hypertension.
- Higher risk in patients with uncontrolled blood pressure.
- Prevalence increases with diabetes and kidney problems.
- Often goes unnoticed without routine eye exams.
Causes of Hypertensive Retinopathy
The main cause of hypertensive retinopathy is chronic high blood pressure. Constant pressure damages and weakens the tiny retinal vessels. This makes them more likely to narrow, leak, or burst over time. Uncontrolled hypertension is the leading factor behind the disease.
Main causes include:
- Chronic hypertension: long-term blood pressure damage.
- Diabetes: raises the risk of blood vessel damage.
- High cholesterol: contributes to the narrowing of vessels.
- Kidney disease: worsens vascular strain.
- Unhealthy habits: smoking and poor lifestyle choices.
Risk Factors for Hypertensive Retinopathy
Not all people with high blood pressure develop hypertensive retinopathy, but certain risk factors increase vulnerability. Poorly controlled blood pressure is the strongest risk. Obesity and lack of exercise contribute to both hypertension and eye vessel damage. Family history of hypertension also raises the likelihood.
Risk factors include:
- Poorly controlled or untreated blood pressure.
- Obesity and lack of physical activity.
- Family history of hypertension or vascular disease.
- Older age (especially above 40).
- Ethnicity, with higher prevalence in African and South Asian populations.
Symptoms of Hypertensive Retinopathy
This condition often shows no symptoms in its early stages. However, as damage worsens, patients may notice blurred or reduced vision. Headaches are also common because of high blood pressure’s impact on eye circulation. In advanced stages, vision may become severely impaired.
Common symptoms include:
- Blurred or reduced vision.
- Persistent headaches.
- Double vision or eye strain.
- Missing areas in vision.
- Sudden vision loss in severe cases.
Complications of Hypertensive Retinopathy
If hypertensive retinopathy is not managed, it can lead to serious complications. One of the most dangerous is retinal vein or artery occlusion, where blood flow to the retina is blocked. Macular edema, or swelling in the central vision area, can also develop. Both can cause severe vision loss.
Potential complications include:
- Retinal vein or artery occlusion.
- Macular edema (central vision swelling).
- Optic neuropathy (damage to the optic nerve).
- Permanent blindness in advanced cases.
- Increased risk of stroke and heart attack.
Treatment for Hypertensive Retinopathy
Treatment focuses on controlling blood pressure and protecting the eyes from additional harm. Medication may be prescribed to stabilize blood pressure levels. Lifestyle changes such as reducing salt, exercising, and quitting smoking are also key. Controlling cholesterol and diabetes lowers the risk of complications.
Treatment options include:
- Blood pressure medications for control.
- Lifestyle changes: diet, exercise, and quitting smoking.
- Cholesterol and diabetes management.
- Laser therapy for sealing leaking blood vessels.
- Regular eye exams for continuous monitoring.
Preventing Hypertensive Retinopathy
Prevention is the best defense against hypertensive retinopathy. The most important step is to control blood pressure through medications and healthy habits. A diet low in salt supports both heart and eye health. Regular exercise helps maintain healthy circulation and vascular strength.
Prevention tips:
- Control blood pressure with regular monitoring.
- Eat a low-salt, balanced diet.
- Avoid smoking and excessive alcohol.
- Exercise regularly to strengthen circulation.
- Get yearly eye exams for early detection.
Protecting Your Vision with Vision Gallery
Hypertensive retinopathy is a silent but dangerous eye condition linked to high blood pressure. Without proper care, it can progress to severe vision problems and even blindness. Fortunately, with timely diagnosis and treatment, the risk of permanent damage can be reduced. Preventive care and ongoing management are key.
At Vision Gallery, we provide advanced diagnostic tools and expert eye disease management to protect your vision. Our specialists focus on personalized care and long-term monitoring. Patients are empowered to take control of their health with our guidance.