Eye floaters are small, shadowy shapes that drift across your field of vision, often resembling dots, squiggly lines, or cobwebs. They are particularly common among individuals as they age and can also occur in specific scenarios, such as floaters after cataract surgery.
Understanding the anatomical changes that lead to floaters is essential, especially for those undergoing cataract surgery co-management to ensure optimal post-surgical care.
So, let’s dive into the causes of floaters, the anatomical changes in the eye that contribute to their formation after cataract surgery, and how they differ from the structure of a healthy eye. Let’s also explore ways to manage floaters effectively.
What Are Eye Floaters?
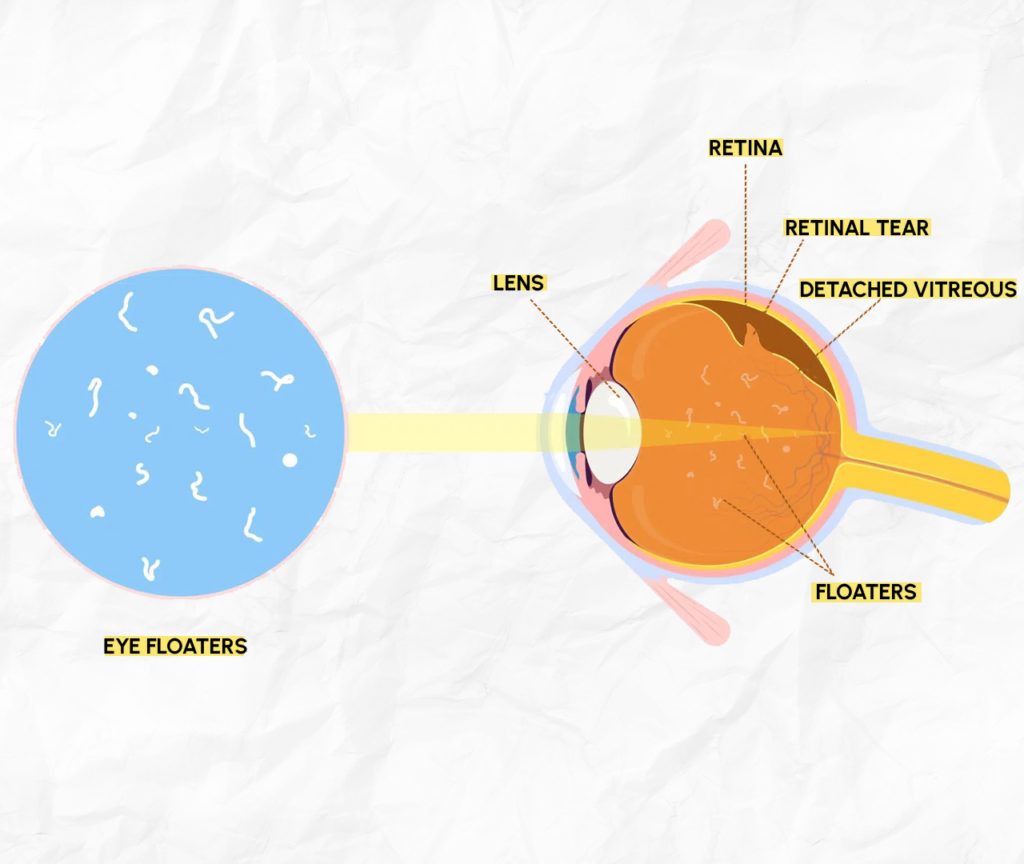
Eye floaters are tiny clumps of collagen or cells that form within the vitreous, a gel-like substance filling the eye. These clumps cast shadows on the retina, causing the perception of floating shapes in your vision.
While generally harmless, floaters can sometimes indicate underlying issues, particularly if they suddenly increase in number or are accompanied by flashes of light.
Anatomy of Floaters: How They Form
To understand floaters, let’s take a closer look at the anatomy of the eye and how it changes over time or due to surgery.
The Normal Anatomy of the Eye
- Cornea: The transparent front layer of the eye that refracts light.
- Lens: Focuses light onto the retina.
- Vitreous Humor: A clear, gel-like substance filling the eye cavity behind the lens.
- Retina: The light-sensitive layer at the back of the eye that processes visual information.
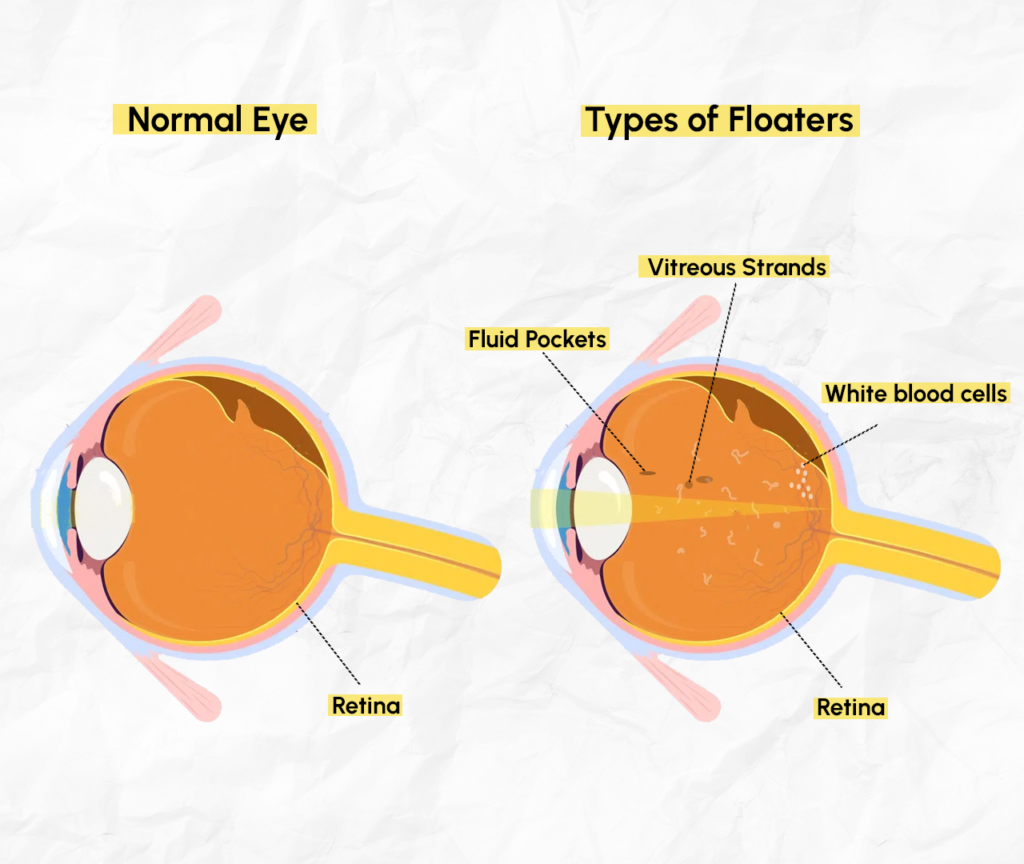
In a healthy eye, the vitreous is well-structured, clear, and evenly gel-like, providing a stable medium for light to pass through.
Changes Leading to Floaters
Over time, the vitreous begins to liquefy, and tiny collagen fibers may clump together. These clumps cast shadows on the retina, appearing as floaters in your vision.
Anatomical Changes After Cataract Surgery
Why Floaters Appear Post-Surgery
- During cataract surgery, the natural lens is replaced with an artificial intraocular lens (IOL). This procedure can disturb the vitreous, potentially causing or exacerbating floaters.
- Post-surgical inflammation may also contribute to the perception of floaters, though these typically resolve over time.
Comparison: Healthy Eye vs Eye With Floaters
Here’s a visual diagram to clarify:
- Healthy Eye
- Vitreous is uniform and clear.
- Light passes directly through to the retina without interference.
- Eye With Floaters
- Clumps or fibers in the vitreous disrupt the path of light, casting shadows on the retina.
- Floaters appear as moving shapes in the visual field.
Common Symptoms of Floaters After Surgery
Floaters are visual phenomena that appear as shadowy shapes drifting across your field of vision, especially after cataract surgery. While they can vary in form and severity, here are some of the most commonly reported symptoms:
- Moving Shapes in Vision
Floaters often appear as dots, squiggly lines, cobwebs, or even thread-like strands that move as your eyes move. They may seem to dart away when you try to focus on them.
- Increased Visibility in Certain Backgrounds
Floaters are most noticeable against bright or uniform backgrounds, such as a clear blue sky, a white wall, or a computer screen. These high-contrast settings make the shadows they cast more prominent.
- Shadows or Streaks That Drift
As floaters are suspended in the vitreous gel of your eye, they may appear to “float” or drift slowly when your eyes stop moving. This phenomenon occurs because the clumps causing the floaters are not fixed and tend to lag slightly behind the movement of your eye.
Diagnosis and Monitoring
Floaters are often detected during a comprehensive eye exam. Your eye doctor may use:
- Dilated Eye Exam: To examine the vitreous and retina.
- Optical Coherence Tomography (OCT): For detailed imaging of the vitreous and retinal layers.
Floaters and Cataract Surgery Co-Management
When undergoing cataract surgery, co-management between your surgeon and optometrist ensures comprehensive care. This collaboration is particularly vital if floaters develop post-surgery.
Role of Co-Management:
- Pre-Surgery Assessment: Your care team evaluates the vitreous and retina to identify pre-existing floaters or risks, enabling a tailored surgical approach.
- Post-Surgery Monitoring: After surgery, your team monitors for new floaters and addresses concerns such as retinal detachment or inflammation.
- Patient Education: You’ll be guided on distinguishing normal floaters from warning signs like flashes of light or a sudden increase in floaters, ensuring prompt action if needed.
This collaborative approach enhances your recovery and long-term eye health while addressing any floaters effectively.
How to Manage Floaters?
Non-Surgical Options
- Observation: Floaters typically become less noticeable over time as the brain learns to ignore them. This natural adjustment often means no medical intervention is necessary for mild cases.
- Lifestyle Adjustments: Avoid looking at bright, blank surfaces like clear skies or white walls, where floaters appear more prominent. Adjusting lighting and contrast in your environment can also help reduce their visibility.
Medical and Surgical Options
- Vitrectomy: This surgical procedure removes the vitreous gel along with the floaters, replacing it with a saline-like solution. It’s effective but generally reserved for severe cases due to potential risks like retinal detachment.
- Laser Therapy: This less invasive option uses lasers to break up larger floaters, making them smaller and less noticeable. It’s an option for patients with moderate floaters who find them disruptive.
Preventive Measures to Take
While floaters cannot always be prevented, you can reduce your risk by:
Manage Chronic Health Conditions
Control underlying conditions such as diabetes, high blood pressure, or autoimmune diseases that can affect eye health.
Protect Your Eyes from Trauma
Wear protective eyewear during sports, construction work, or any activity that poses a risk of eye injury.
Stay Hydrated
Proper hydration supports overall eye health and may help maintain the vitreous gel’s consistency.
Follow a Healthy Diet
Include foods rich in antioxidants, vitamins A, C, and E, and omega-3 fatty acids to support eye health and prevent early aging of the eye structures.
Quit Smoking
Smoking accelerates oxidative stress, increasing the risk of eye conditions, including vitreous degeneration.
Limit Screen Time
Take regular breaks from screens to reduce eye strain, which can exacerbate the perception of floaters.
Monitor Eye Changes
Pay attention to any sudden changes in your vision, such as an increase in floaters, flashes of light, or a shadow in your peripheral vision.
Attend Regular Eye Exams
Early detection of vitreous changes or other eye issues can help address problems before they escalate.
Maintain a Healthy Weight
Excessive weight can contribute to systemic conditions like diabetes, which may indirectly impact your eye health.
Vision Gallery’s Expertise in Cataract Surgery Co-Management
If you’re experiencing floaters or preparing for cataract surgery, the team at Vision Gallery offers expert care through every step of the process. Our approach to cataract surgery co-management ensures a smooth journey from pre-surgery evaluation to post-surgery monitoring. Floaters after cataract surgery are manageable with proper care. Trust Vision Gallery to provide the expertise and support you need for healthy, clear vision. Call us for an appointment today, dial 281-377-0219.